CURRENT PROJECTS
Ongoing research in the Bergen Research Group for UltraSound in GastroEnterology (BRUSE) includes:
Main content
SonoDOCc: Utilizing ultrasound contrast agents in Crohn's disease
In recent times, ultrasound has been recognised as an essential part in the follow-up and diagnosis of patients with Crohn's, and the medical department at HUH, in collaboration with NCUG, has extensive expertise in this area. However, there are limitations associated with the current survey method. The project therefore aims to develop a new method with ultrasound to better visualize disease changes in the terminal ileum
Contact: Kim Nylund
Gastric dysmotility and visceral hypersensitivity - an ultrasound approach to functional GI disorders
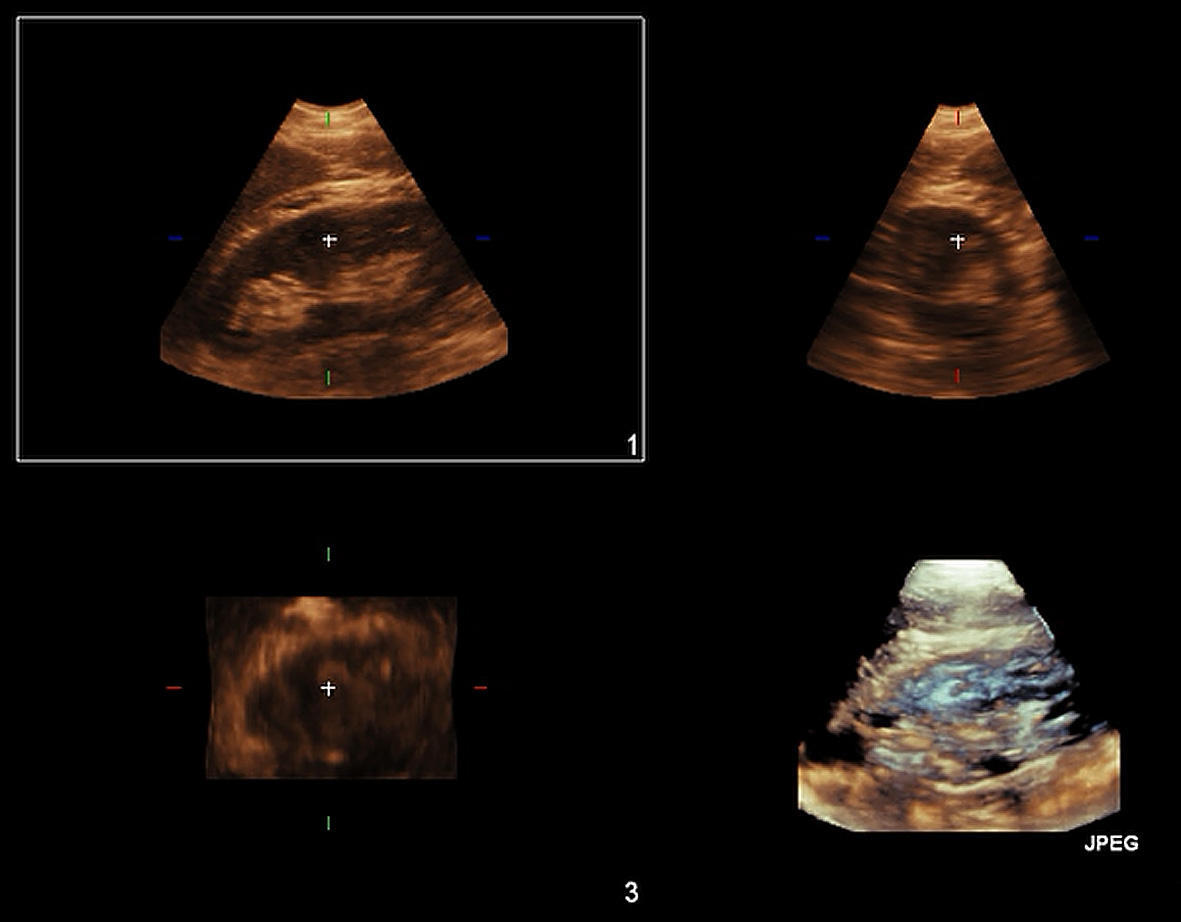
The aim of Dr. Steinsvik’s team is to explore commonalities between chronic fatigue syndrome (ME / CFS) and functional gastrointestinal disorders such as functional dyspepsia (FD) and irritable bowel syndrome (IBS). This is done mainly by examining the stomach in connection with a soup meal using an ultrasound function examination (Ultrasound Meal Accommodation test or ULFU).
Research focus
Ultrasound function examination (ULFU) is a clinical examination in which several factors are studied at once in a non-invasive, harmless and affordable procedure. Recording the amount of symptoms the patient experience by drinking 500 ml of broth, provides information about the degree of visceral hypersensitivity. In addition, the patient completes a survey of which meal-related symptoms are most prominent. By using the broth as a contrast fluid in the stomach, the team can then study the stomach's ability to expand in response to the meal ("accommodation capacity"), the distribution of fluid between the upper and lower part of the stomach, in addition, an indication of the stomach’s ability to empty. An important sub-project has been to collect normal material for ULFU to create reference values for the test. This is useful for all subprojects in the study.
Projects and important results
This project studies how different patient groups respond to this ultrasound examination, but has also compared ultrasound function examination with scintigraphy, the gold standard method of gastric emptying. The team has found that ULFU provides valuable information about both symptoms and dysmotility in more patient groups than have previously been mapped. Furthermore, that enlarged antrum in the fasting state, and dilation of the proximal stomach 20 minutes after consuming low-calorie soup is associated with delayed gastric emptying measured by conventional methods. The team conclude that this ultrasound method contributes to increased knowledge about the individual patient that can improve treatment and guide further investigation, and thus facilitate personalized treatment for these complex disorders.
Contact: Elisabeth Kjelsvik Steinsvik
Relapse of Ulcerative colitis diagnosed by ultrasonography
The aim of Dr. Nylund’s team is to investigate whether ultrasound measurements can predict endoscopic recurrence in patients with ulcerative colitis.
Research focus
Ulcerative colitis is an inflammatory disease of the intestine with a variable course. It is important to be able to diagnose a relapse early to adjust the medical treatment. Currently, ileocolonoscopy is the best tool, but the examination is invasive and should be replaced by a method that is more agreeable to patients. Ultrasound of the bowel can be such a method. The PRELAPSE study should include ulcerative colitis patients who have been treated with an anti-TNF drug for a year or longer and who have been disease-free for the past 3 months. The same patients are already being recruited in another study (BIOSTOP). The aim of the study is to investigate whether ultrasound measurements can predict endoscopic recurrence in patients in persistent clinical and endoscopic remission. It is a longitudinal, exploratory, observational study.
Contact: Kim Nylund
Sonorescue: selecting patients with severe ulcerative colitis for rescue therapy using ultrasonography
The aim of Dr. Nylund’s team is to identify patients with acute severe ulcerative colitis in need of “rescue” therapy by repeated ultrasound examinations during hospitalization.
Research focus
Acute severe ulcerative colitis (ASUC) is a medical emergency that requires hospitalization and prompt treatment with intravenous corticosteroids. Unfortunately, 1/3 of the patients do not respond to this treatment and need so-called "rescue" treatment. This is a clinical decision, but repeated ultrasound examinations of the bowel can be used to distinguish responders from non-responders. The primary endpoint of this prospective, longitudinal observational study of 90 patients with ASUC is "rescue" treatment due to insufficient efficacy of iv corticosteroids. The study involves repeated examinations of the patient, but three of these can be performed during hospitalization. A faster and better selection of patients for "rescue" treatment can improve the outcome of the treatment, but also reduce costs.
Contact: Kim Nylund
Sonoporation-enhanced treatment of inoperable pancreatic cancer
Our team, led by Prof. Dimcevski, aims to study the safety and efficacy of sonoporation combined with chemotherapy for patients with inoperable pancreatic cancer. We hypothesize that the combined treatment will result in improved survival without increasing systemic toxicity.
Pancreatic cancer is the seventh most common cause of cancer death in both men and women worldwide, with more than 450,000 new cases in 2018. With a mortality-to-incidence ratio of 0.94 and five-year survival rates at around 8.5% (1, 2), pancreatic cancer is a diagnosis dreaded by both clinicians and patients, and advances in treatment options are warranted. When treating pancreatic ductal adenocarcinoma (PDAC), the tumour’s response to chemotherapy is notoriously very low. This is caused by a dense desmoplastic stroma and poor blood supply in and around the tumour (3, 4) albeit, perfusion is sufficient to observe substantial signals in contrast-enhanced ultrasound (5). Regardless of the curative intent of treatment for patients who present with surgically amenable PDAC and undergo resection followed by adjuvant chemotherapy, their median overall survival is still only 15 months (6, 7).
Sonoporation is a novel technique that uses ultrasound and ultrasound contrast agents (microbubbles) to enhance the therapeutic efficacy of a given drug at a localised area. When ultrasound waves reach the microbubbles, they oscillate, and through a range of mechanisms, sonoporation allow for increased drug delivery and tissue sensitisation in the targeted area, i.e., the tumour. Taking into account that a major drawback to traditional chemotherapy is the systemic toxic side effects, especially when used in high therapeutic concentrations, sonoporation may provide an effective solution.
In this open, randomized, single-center clinical trial, we will study the safety and efficacy of sonoporation combined with standard of care chemotherapeutic regimens (Gemcitabine and Nab-Paclitaxel, or FOLFIRINOX). All patients will receive standard of care chemotherapy, and through randomization, patients will be allocated to either sonoporation or control. Patients in the sonoporation groups will undergo 30 minutes of treatment with microbubbles (SonoVue) and targeted ultrasound in addition to the chemotherapy. We hypothesize that the sonoporation group will have increased median survival, be able to undergo more treatment cycles and maintain a high quality of life - without increased side effects. The techniques being developed through the study may have major consequences both for this patient group, but also for patients with other solid cancers where the treatment may prove relevant.
References
1. Bray F et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin (2018). 2. Reichman M et al. SEER Cancer Statistics Review, 1975-2005. SEER Cancer Statistics Review (2008). 3. Provenzano PP et al. Enzymatic targeting of the stroma ablates physical barriers to treatment of pancreatic ductal adenocarcinoma. Cancer Cell (2012). 4. Tod J et al. Tumor-stromal interactions in pancreatic cancer. Pancreatology (2013). 5. Kotopoulis S et al. Treatment of human pancreatic cancer using combined ultrasound, microbubbles, and gemcitabine: a clinical case study. Med Phys (2013). 6. Riall TS et al. Pancreaticoduodenectomy with or without distal gastrectomy and extended retroperitoneal lymphadenectomy for periampullary adenocarcinoma--part 3: update on 5-year survival. J Gastrointest Surg (2005). 7. Chen EL et al. Long-term survival after pancreatic cancer treatment. Am J Surg (2007)
Contact: Odd Helge Gilja and Ingrid Kvåle Nordaas
Optimizing Ultrasound Enhanced Delivery of Therapeutics: A Randomized Clinical Trial in Patients With Inoperable Pancreatic Cancer
In this multicenter clinical trial, we aim to study the safety and efficacy of sonoporation combined with chemotherapy for patients with inoperable pancreatic cancer. We hypothesize that the combined treatment will result in improved survival without increasing systemic toxicity.
Pancreatic cancer is the seventh most common cause of cancer death in both men and women worldwide, with more than 450,000 new cases in 2018. With a mortality-to-incidence ratio of 0.94 and five-year survival rates at around 8.5% (1, 2), pancreatic cancer is a diagnosis dreaded by both clinicians and patients, and advances in treatment options are warranted. When treating pancreatic ductal adenocarcinoma (PDAC), the tumour’s response to chemotherapy is notoriously very low. This is caused by a dense desmoplastic stroma and poor blood supply in and around the tumour (3, 4) albeit, perfusion is sufficient to observe substantial signals in contrast-enhanced ultrasound (5). Regardless of the curative intent of treatment for patients who present with surgically amenable PDAC and undergo resection followed by adjuvant chemotherapy, their median overall survival is still only 15 months (6, 7).
Sonoporation is a novel technique that uses ultrasound and ultrasound contrast agents (microbubbles) to enhance the therapeutic efficacy of a given drug at a localised area. When ultrasound waves reach the microbubbles, they oscillate, and through a range of mechanisms, sonoporation allow for increased drug delivery and tissue sensitisation in the targeted area, i.e., the tumour. Taking into account that a major drawback to traditional chemotherapy is the systemic toxic side effects, especially when used in high therapeutic concentrations, sonoporation may provide an effective solution.
In this open, randomized, multicenter clinical trial, we will study the safety and efficacy of sonoporation combined with standard of care chemotherapeutic regimens (Gemcitabine and Nab-Paclitaxel, or FOLFIRINOX). All patients will receive standard of care chemotherapy, and through randomization, patients will be allocated to either sonoporation or control. Patients in the sonoporation groups will undergo 20 minutes of treatment with microbubbles (Sonazoid) and targeted ultrasound in addition to the chemotherapy. We hypothesize that the sonoporation group will have increased median survival, be able to undergo more treatment cycles and maintain a high quality of life - without increased side effects. The techniques being developed through the study may have major consequences both for this patient group, but also for patients with other solid cancers where the treatment may prove relevant.
References
1. Bray F et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin (2018). 2. Reichman M et al. SEER Cancer Statistics Review, 1975-2005. SEER Cancer Statistics Review (2008). 3. Provenzano PP et al. Enzymatic targeting of the stroma ablates physical barriers to treatment of pancreatic ductal adenocarcinoma. Cancer Cell (2012). 4. Tod J et al. Tumor-stromal interactions in pancreatic cancer. Pancreatology (2013). 5. Kotopoulis S et al. Treatment of human pancreatic cancer using combined ultrasound, microbubbles, and gemcitabine: a clinical case study. Med Phys (2013). 6. Riall TS et al. Pancreaticoduodenectomy with or without distal gastrectomy and extended retroperitoneal lymphadenectomy for periampullary adenocarcinoma--part 3: update on 5-year survival. J Gastrointest Surg (2005). 7. Chen EL et al. Long-term survival after pancreatic cancer treatment. Am J Surg (2007)
Contact: Georg Dimcevski, Odd Helge Gilja and Ingrid Kvåle Nordaas
New diagnostics and treatment of diabetic gastroparesis
Contact: Dag André Sangnes
The PanGut study, work package: gastrointestinal hormonal responses and gall bladder emptying
Contact: Eirik Søfteland
Intestinal fluid balance and inflammation in experimental ETEC infection
Contact: Hilde Løland von Volkmann
Minimal invasive endoscopic procedures for diagnosis and treatment of esophageal motility disorders
Contact: Khanh Do-Cong Pham
Ultrasound-enhanced delivery of chemotherapeutic drugs to cancer patients
Contact: Spiros Kotopoulis
Improving diagnostics and building a new scoring system for chronic pancreatitis based on Bergen multimodal pancreas database.
Contact: Trond Engjom