Blood sample 24 hours after start of chemotherapy predicts survival
Acute myeloid leukemia is an aggressive blood cancer with poor survival. Younger and otherwise healthy patients undergo severe chemotherapy, often accompanied by stem cell transplant, even though it is difficult to predict who will benefit from the treatment. Now, a simple blood test can measure whether the patient's cancer will respond to chemotherapy. If the chemo has no effect, critical weeks are gained to find the right treatment.

Main content
Quickly determining responsiveness
Although high rates of initial chemotherapy response, patients often relapse due to the selection and development of chemotherapy-resistant leukemic cells.
"When treating patients with leukemia, it is challenging to quickly follow whether the patient is responding to therapy or not. The response to therapy is currently measured after weeks to months of treatment, thereby losing important time. This could result in weeks of non-functional and harsh treatment for the patient, and loosing valuable time that could have been used for targeted and functional therapy," Benedicte Sjo Tislevoll explains, PhD candidate at CCBIO and the Department of Clinical Science, UiB, and first author of this study.
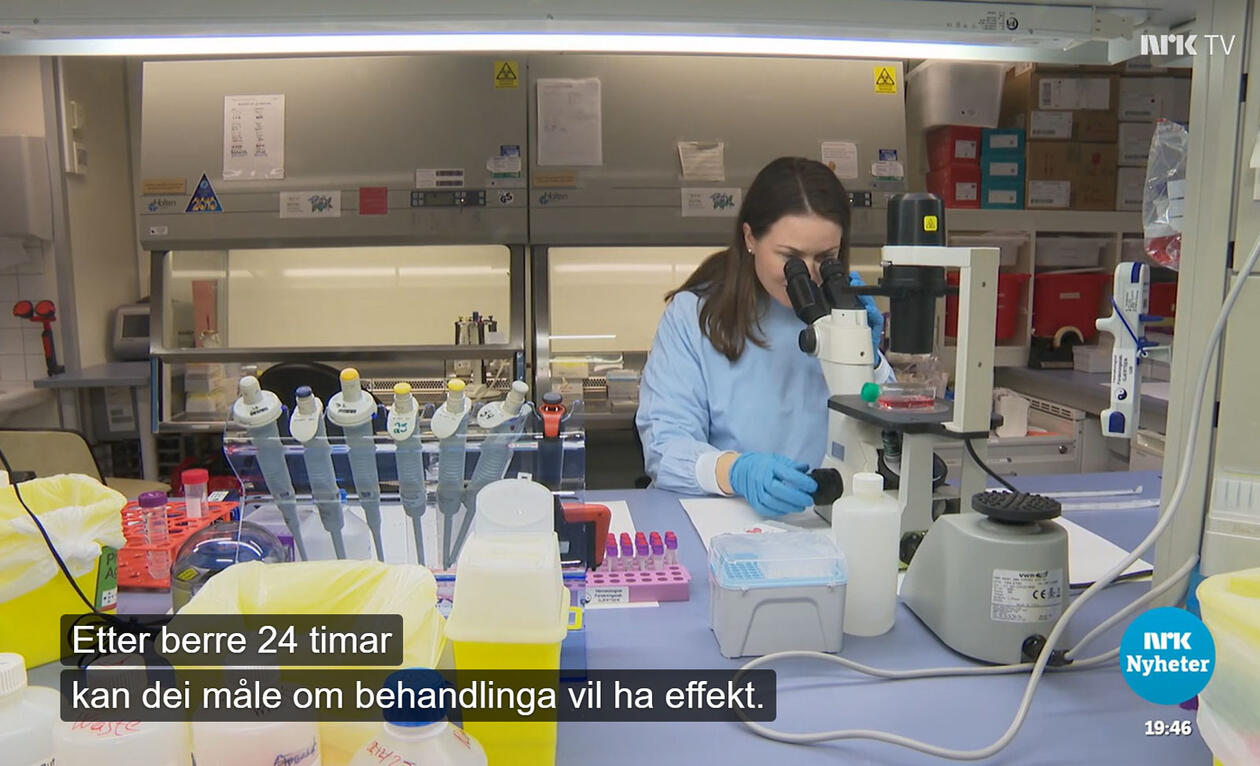
However, an immediate response to chemotherapy can be measured by investigating the functional properties of the leukemic cells. Tislevoll has in her doctoral work been investigating whether measurements during the first 24 hours of chemotherapy can predict the patient's long term response to the treatment. She has been investigating cell signaling proteins in blood samples taken before and 4 and 24 hours after startup of chemotherapy.
More targeted treatment
Tislevoll's work shows that the signal of phosphorylated ERK1\2 increases within the first 24 hours of chemotherapy in patients who have a poor response to chemotherapy.
"We believe that this protein is responsible for the cancer cells’ resistance to chemotherapy and can be used to distinguish responders from non-responders. It can also show us how the cancer cells protect itself against the chemotherapy. This can be an important key in our understanding of cancer, and our aim is to use this information to change treatment early for patients who are not responding to therapy. Hopefully we can use this for several types of leukemia, and also translate the principle to other cancers," Tislevoll concludes.
Media attention
See news story on NRK Vestlandsrevyen and NRK Dagsrevyen fra 12.01.23, and BT 13.01.23 (all in Norwegian). Also see LabMedica og AlphaGalileo.
The research is published in the high impact journal Nature Communications, in the article Early response evaluation by single cell signaling profiling in acute myeloid leukemia. This is paper 1 in Tislevoll's doctorate work. Main supervisor has been Professor Bjørn Tore Gjertsen, and co-supervisor has been researcher Monica Hellesøy.