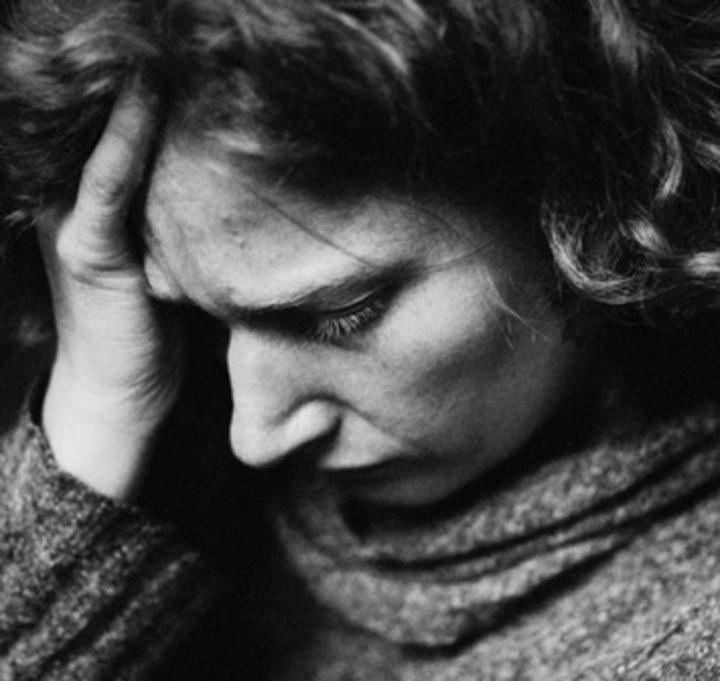
Diabetes and depression- a common connection
In this recently published article, Line Iden Berge takes a closer look at depressive disorders in persons with type 1 diabetes.
Main content
Prevalence and characteristics of depressive disorders in type 1 diabetes
Berge LI, Riise T, Hundal O, Odegaard KJ, Dilsaver S,
Lund A. BMC Res Notes.2013 Dec 19
Both Diabetes 1 and depression are common diseases in the general population, and persons with diabetes and depression actually have an increased risk of complications and also increased mortality. This factor has led the American Diabetes Association to recommend screening for depression, anxiety and psychosocial problems as a part of the medical management of diabetes.
This study, recently published in BMC Research Notes, was designed to ascertain the frequency and clinical characteristics of depressive disorders in a group of persons with type 1 diabetes. To further investigate the impact of depressive disorders in diabetes, PhD candidate Line Iden Berge and her colleagues compared the glycosylated haemoglobin levels between the groups of persons with ongoing and/or previous depressive disorders to those without depressive disorders.
Associations between diabetes and depressive disorders – a study
In total, 51 consecutive patients attending a routine control at the hospital were included in the study. Psychiatric diagnoses were assessed using five modules included in the Mini International Neuropsychiatric Interview (M.I.N.I), Norwegian Version 5.0.0, part A (ongoing or previous major depressive episode, major depressive episode with melancholia), part B ( dysthymia), part D (mania/hypomania) and part E (panic attacks). Differences in glycosylated haemoglobin (HbA1c) between groups of persons with and without depressive disorders were estimated using linear regression models adjusting for sex, age and duration of diabetes.
According to M.I.N.I 17 persons (33%) were diagnosed with either an ongoing major depressive episode, ongoing dysthymia or previous depressive episode(s). Eight persons were in the midst of a major depressive episode, of these, 7 met the criteria for melancholia. A high prevalence of self-reported family history of depressive disorders were found, even among those who did not have a history of depressive disorders themselves. Persons with depressive disorders had higher HbA1c levels than those without depression, although the difference was not significant possibly due to the rather small sample
A high prevalence of melancholic depression:
The results are in accordance with other studies within the field, suggesting that as many as one sixth of persons with type 1 diabetes may suffer from a current major depressive episode. Interestingly, the result also showed a high prevalence of melancholic depression, often considered a more severe and “biologic” type of depression with anhedonia and psychomotor retardation as core features. As depression in in persons with diabetes is associated with increased risk of complications and increased mortality, and that melancholic depression is more severe, the clinicians should pay more attention to this group.
Future studies should examine prevalence and clinical characteristics of depressive disorder using a larger sample, and especially focus on the high prevalence of melancholic depression among persons with type 1 diabetes.