Susanna Myrnerts Höök: Helping Neonates Survive the First Day of Life
Susanna Myrnerts Höök is a Paediatric Specialist from the Sachs' Children and Youth Hospital, Stockholm, Sweden. The last 4 years she has been involved in research projects focusing on neonatal resuscitation in Kampala, Uganda, a low-resource setting. The work led her to start a PhD September 2016.

Main content
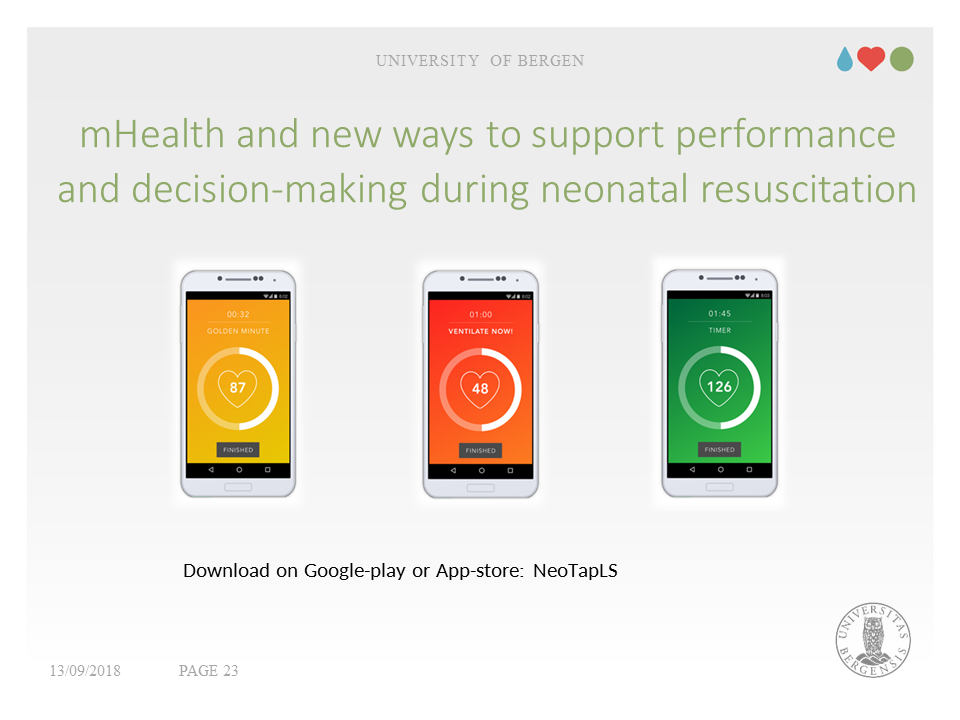
Myrnerts Höök’s PhD project is entitled, “mHealth and New Ways to Support Performance and Decision-making during Neonatal Resuscitation”.
The “Golden Minute”
The "Golden Hour" of neonatal life is defined as the first hour of post-natal life. It is based on the first critical hour concept in adult trauma situations. For neonates, however, every minute is important. Within one minute of birth, a baby should be breathing well or should be ventilated with a bag and mask. The “Helping Baby Breathe” (HBB) programme has adopted the Golden Minute as its credo. HBB identifies the steps that a birth attendant must take immediately after birth to evaluate the baby and stimulate breathing.
Breathing = Survival
Successful resuscitation could prevent a large proportion of early neonatal deaths (first week of life) and could improve the outcomes of neonates surviving birth asphyxia. A number of programmes focus on neonatal survival issues in resource-limited settings. The HBB programme emphasizes skilled attendance at birth and basic newborn care. The cornerstone of its training is to teach appropriate ventilation skills.
Providing effective positive pressure ventilation is the single most important component of successful neonatal resuscitation. A correct ventilation rate can be managed using a bag and mask, or by using a laryngeal mask, which is a supraglottic airway device that keeps a patient's airway open during anaesthesia or resuscitation.
Myrnerts Höök and another CIH PhD student, Nicolas Pejovic, are researchers in a large clinical trial comparing the 2 ventilation methods. The trial, Neonatal Resuscitation with Supraglottic Airway Trial (NeoSupra trial), is led by Myrnerts Höök’s PhD supervisor, Professor Thorkild Tylleskär. Learn more about NeoSupra.
Assessing heart rate is critical
Accurately assessing the heart rate provides essential feedback on the quality of the ventilation. Heart rate can be determined by auscultating the precordium, or by palpating the umbilical cord. Improved ventilation and calls for help are recommended if the heart rate is <100 beats per minute.
Unfortunately, in many low- and middle-income settings, neonatal resuscitation is frequently performed by health personnel with limited experience and training in airway management. In addition, these settings lack reliable monitoring equipment. If the equipment is present, the available staff may be inadequately trained in its use.
Working around equipment limitations.
Globally, wireless technology is expanding to even the remotest parts of the world. Nature writes that 95% of the world has mobile-phone coverage and technical experts project that between 36 and 55% of the global population will be using smartphones in 2018.
Although neonatal resuscitation equipment and devices are included in the list of commodities prioritised by the UN commission on life-saving commodities for women and children, sufficient numbers of adequately trained staff in low-resource settings are a problem, even if the priority equipment can be delivered to these areas.
Myrnerts Höök and colleagues at CIH, Sachs’ Children and Youth Hospital, and Karolinska Institute have developed a smartphone application, NeoTapLifeSupport (NeoTapLS), that can be used to accurately and rapidly assess neonatal heart rates. It is a globally accessible, easy-to-use, mobile health system that could be a low-cost alternative to expensive medical equipment. Myrnerts Höök’s first paper piloted the phone app with a group of 30 participants from a variety of backgrounds, using a manikin. The results showed that heart rates could be accurately and rapidly assessed using the mHealth tool, NeoTapLS on mobile phones.
Myrnerts Höök’s PhD project
The aim of Myrnerts Höök’s PhD project is to explore whether the introduction of a new mHealth tool can facilitate the adherence to neonatal resuscitation guidelines in low resource settings. Her various studies will explore whether the tool can support accurate heart rate assessment. She will also go deeper into the background and will look at how neonatal resuscitation is performed today in low resource settings. She will explore midwives’ own perceptions about neonatal resuscitation, specifically focusing on what they think they need to be able to perform their best, and to save lives.
Her studies range from a pilot study of NeoTapLS on manikins (Paper 1 – published), to field work with NeoTapLS, to aspects of midwifery in low-resource settings, including adherence to guidelines, perceptions and knowledge. A number of papers are planned to present the research results; three will be included in the PhD:
- Paper I: Accurate and fast neonatal heart rate assessment with a smartphone-based application- a manikin study
- Paper II: NeoTapLS- a new smartphone-based applications for support when performing neonatal resuscitation in low- income settings
- Paper III: Neonatal resuscitation: a qualitative study on midwives´ perception and knowledge at Mulago Hospital, Uganda
Additional papers to be published after her dissertation:
- Midwifes adherence to the Helping Babies Breathe guidelines at Mulago Hospital in Uganda
- NeoTapLS assisted heart rate assessments versus ECG during neonatal resuscitation in a low-resource setting
- Neonatal Resuscitation with Supraglottic Airway Trial (NeoSupra trial)